Custom Report Store
Welcome to the Ero Health Report Store
Demonstrating how to use data to drive your business if one of the many expertise’s our team at Ero Health has acquired. This comes from years of supporting medical practices using eClinicalWorks® and building custom reports to fit their unique needs.
With this knowledge, we offer a library of commonly requested reports that you can purchase and implement in your database.
If you don’t see what you’re looking for, email us and we can discuss the development of custom reports that meet the individual needs of your practice.
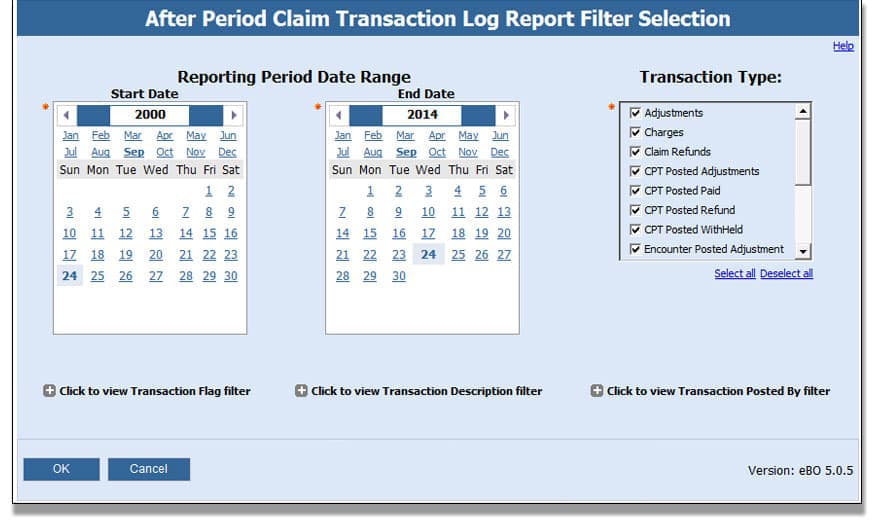
After Period Claim Transaction Log
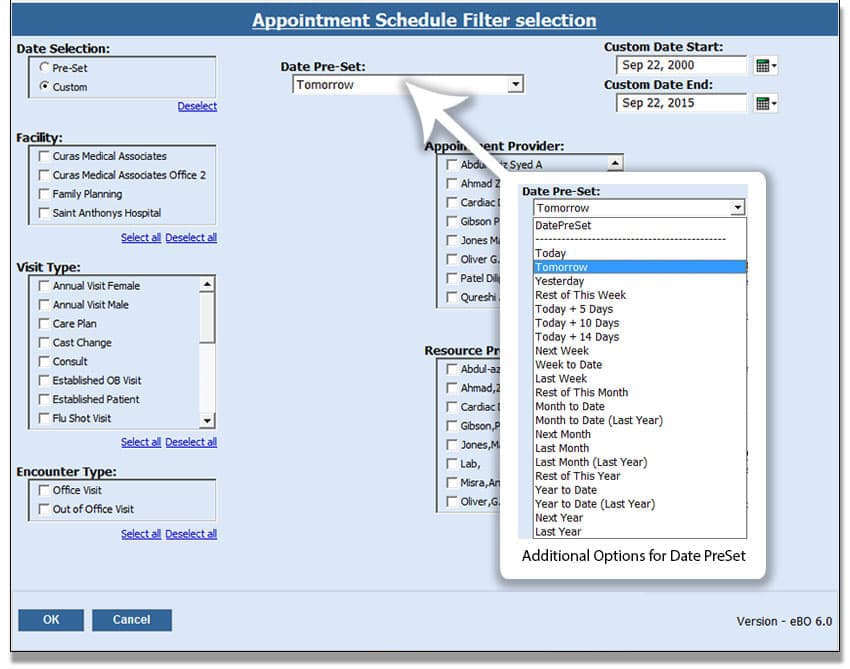
Appointment Schedule
This report is designed to create lists of upcoming or past appointments and can include a list of patient and appointment information; including date, time, reason for visit, general notes, and balances.
This general purpose report is useful in many ways. Help schedule your providers, create checklists for Insurance or Rx eligibility, review patient balances, and more.
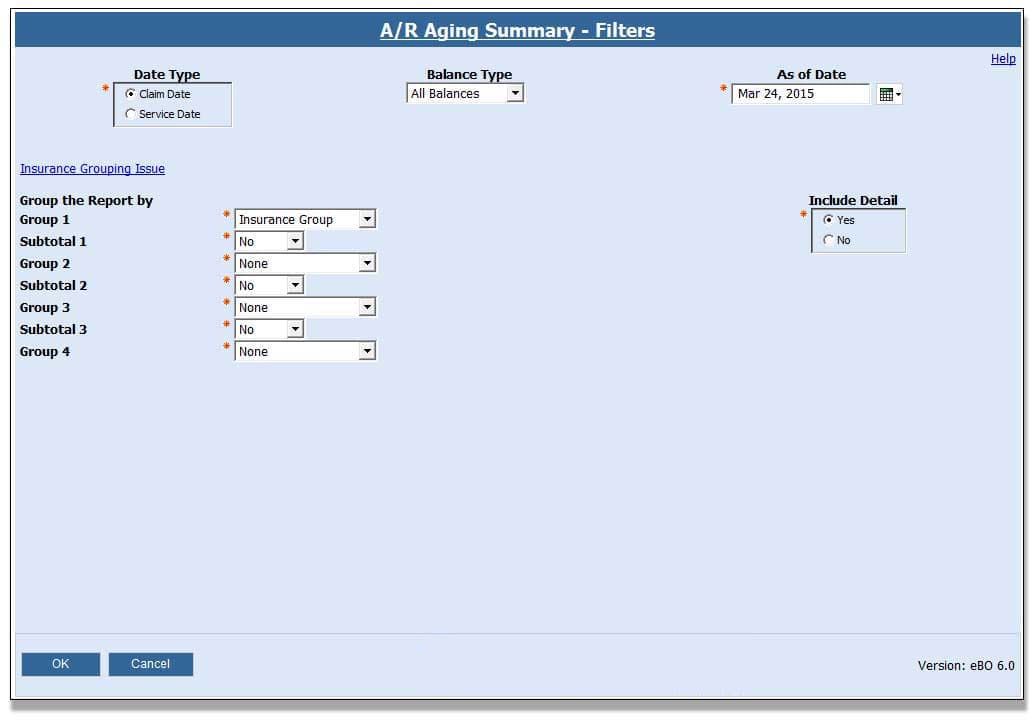
AR Aging Summary
This purpose of this report is to create ‘back in time’ AR reports that balance to the daysheet reports.
This eBO report allows practices with eClinicalWorks® to generate the accounts receivable report as of a particular date. The practice is able to run this report and reconcile against the day sheet summary for a given date range. It can be run by claim date or service date and includes detailed claim information along with unposted payments and refunds.
$450.00
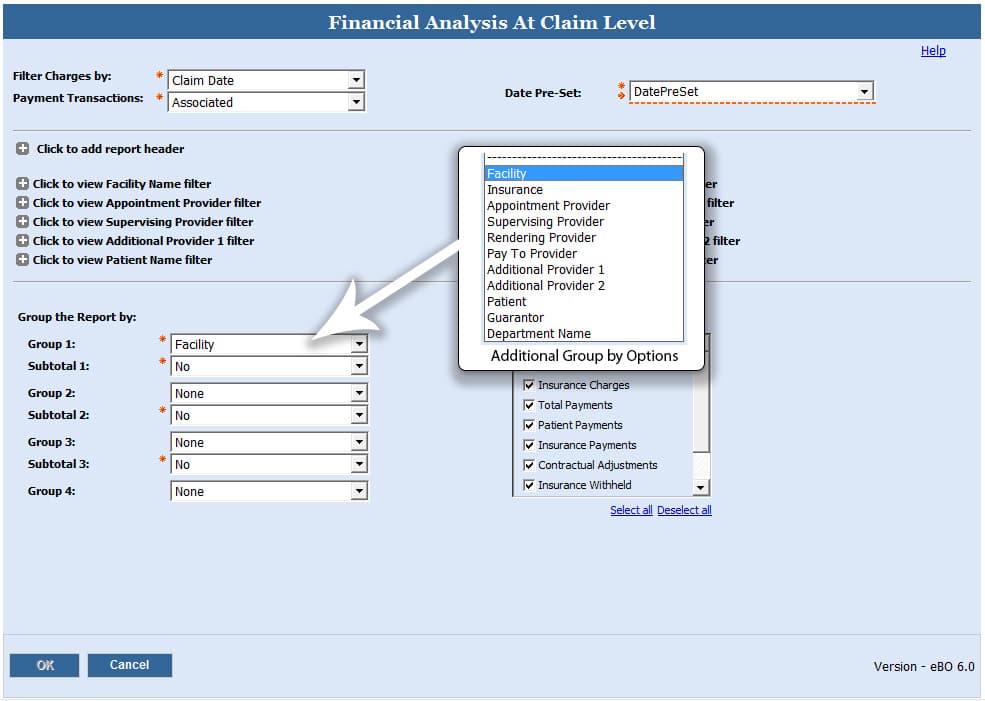
Automated Financial Analysis at Claim Level
This eBO report works as Financial Analysis at Claim Level Report (364). It can be used to automate any of the views created from this report such as the Day Sheet Summary or Charge-Payment Summary reports. This can save a practice a tremendous amount of time at month end since most of the monthly reports that practices use are based off of the Financial Analysis at Claim Level Report.
$450.00
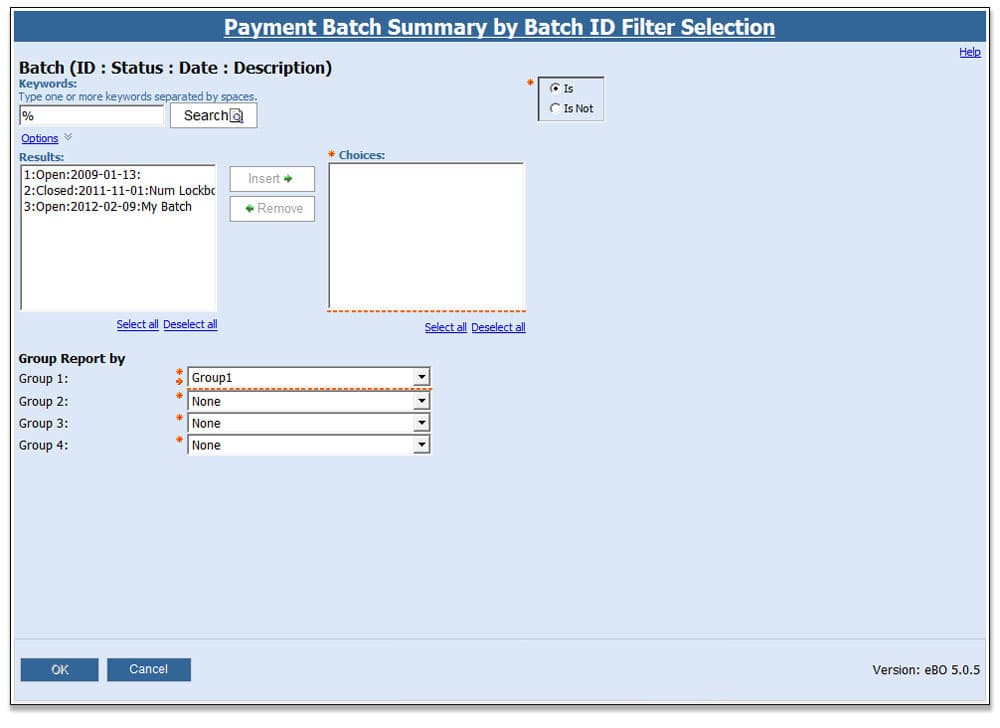
Batch Payment Report
This report is a must have for anyone that uses the Payment Batches in eClinicalWorks®. The Batch Payment Reports were designed to accommodate both payment posters and managers working in practices that use batches to track and manage payments. The Payment Batch Summary by Date report is designed for both managers and payment posters. It can be used to report on batches entered on a given day by person and payment type. The other three reports (by Batch ID, Check Number and Payment ID) are useful for researching payment reconcilement issues.
$250.00
Biller Productivity Report
$500.00
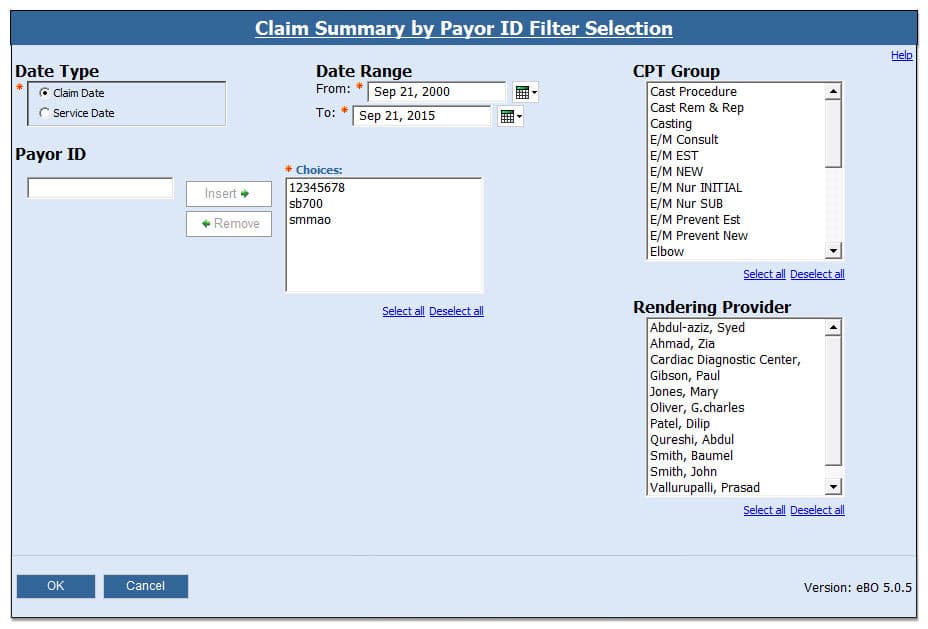
Claim Auditing Reports
This report is helpful if you are having difficulty completing financial audits or struggling to identify report discrepancies. It includes a summary and detailed claims information by Payor ID or Payor Name.
These four reports allow a practice to create detail and summary reports of claims associated to specific providers. This can be useful when auditing month end reports or troubleshooting report discrepancies.
$250.00
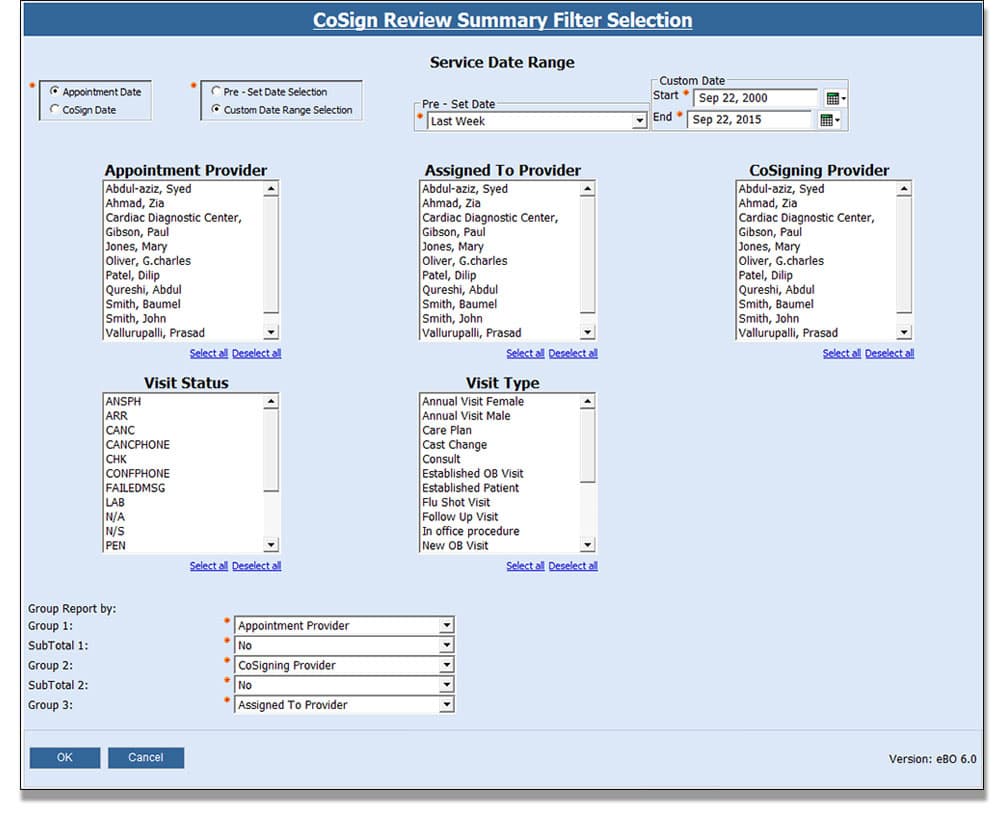
Co-Sign Review
This report is helpful if you have a Document/Monitor CoSign workload. It includes a summary and detailed information on progress notes and appointment, assigned to and cosigning providers.
Make sure that Reviewing and Reviewed Providers are meeting goals in the summary report and drill-down (or run the detail report directly) to see Progress Notes’ details.
$250.00
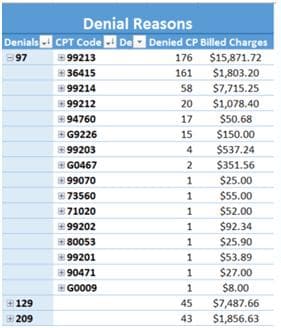
Ero Health Denial Dashboard
Denial management is crucial maximizing your practice’s collection efforts. Analyzing denials is made easy with the Ero Health Denial Dashboard. View a trend of denied claims, number of denied CPT codes, and denial rate for up to 6 months.
$800.00
Ero Health KPI Dashboard
The Ero Health KPI Dashboard is designed to combine several reports run in eBO into a dashboard that provides a monthly snapshot of activity as well as historical trends. In addition, the dashboard displays cancelation and no-show trends, charges and payments by provider, encounters without claims, aging tables and credits, unposted payment trends, and a summary of write-offs over the last year.
View up to 24 months of historical financial information including built-in net collection rates, gross collection rates, and days A/R calculations.
$3,000.00

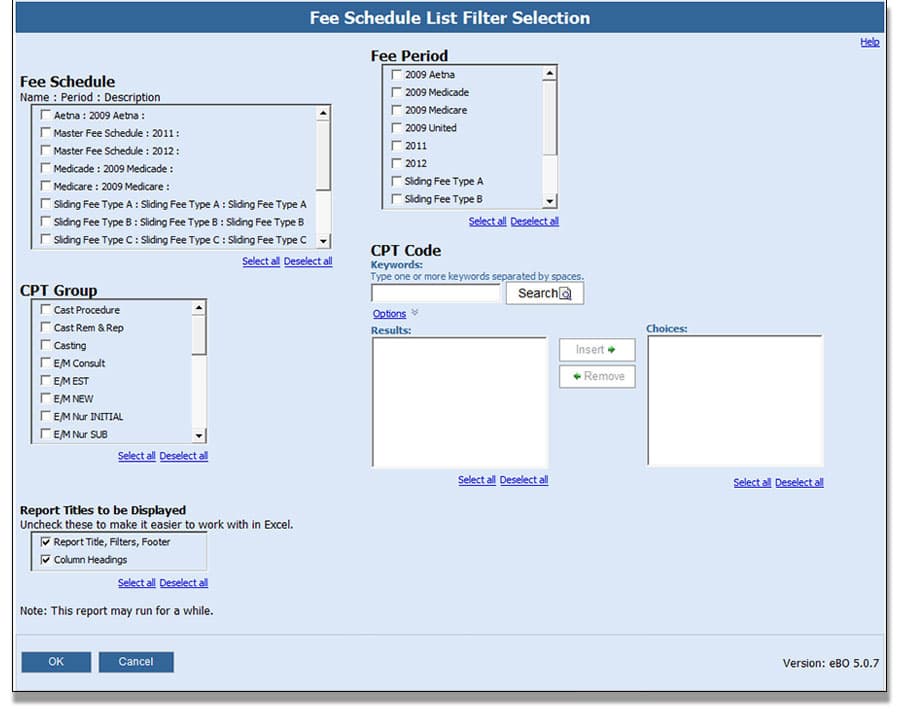
Fee Schedule Listing
This report is helpful if you need to document or list fee schedule(s) and/or compare CPT Codes/Groups across fee schedules. It lists detailed fee schedule information; including name, period, start/stop dates, fee, allowed, cost, etc. by schedule, period for CPT codes or groups.
$250.00
Follow Up Appointment Report
Does your office have a difficult time tracking the scheduling of follow-up visits? This report looks for encounters that have a Follow Up indicated on the progress note and returns whether or not an appointment has been made. Detail includes patient demographic information, the past appointment date, when the follow-up should take place according the progress note, follow-up visit type and date, as well as any future appointments scheduled for the patient.
$500.00

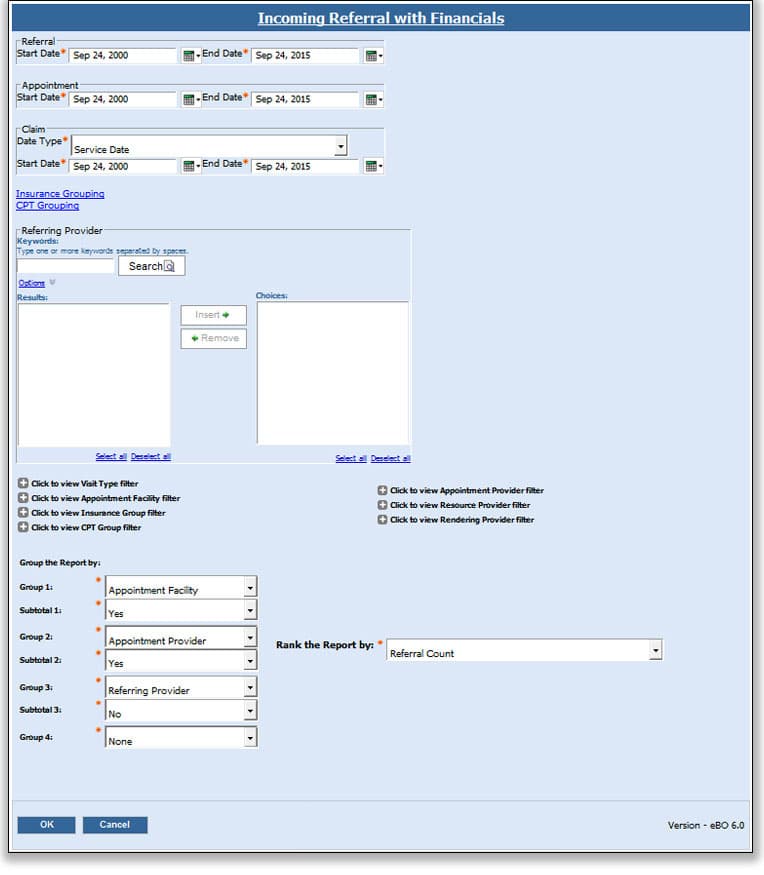
Incoming Referrals with Financials
This report is helpful if you need to know who’s referring patients to you and measure the value based on incoming referrals, summary referral, appointment and claim counts as well as claim billed charges and payments.
$250.00
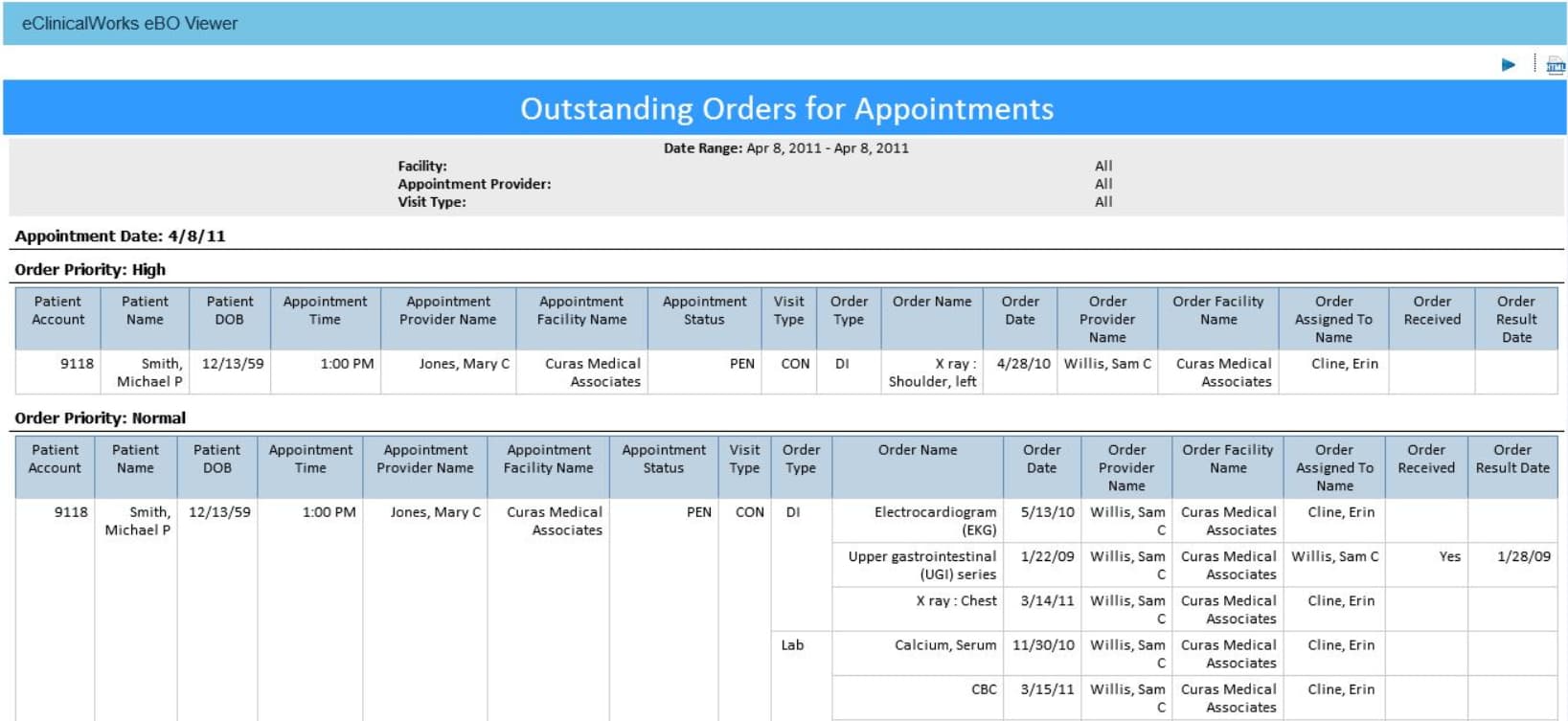
Outstanding Orders for Appointments eBO Report
Managing orders can be a challenge. Whether it’s tracking outstanding orders to verifying that orders have been resulted, there’s no easy and efficient way to ensure that nothing has been missed. With the Outstanding Orders eBO report, users will be able to view outstanding orders for patient with upcoming appointments and patients with orders that have not been resulted.
$500.00
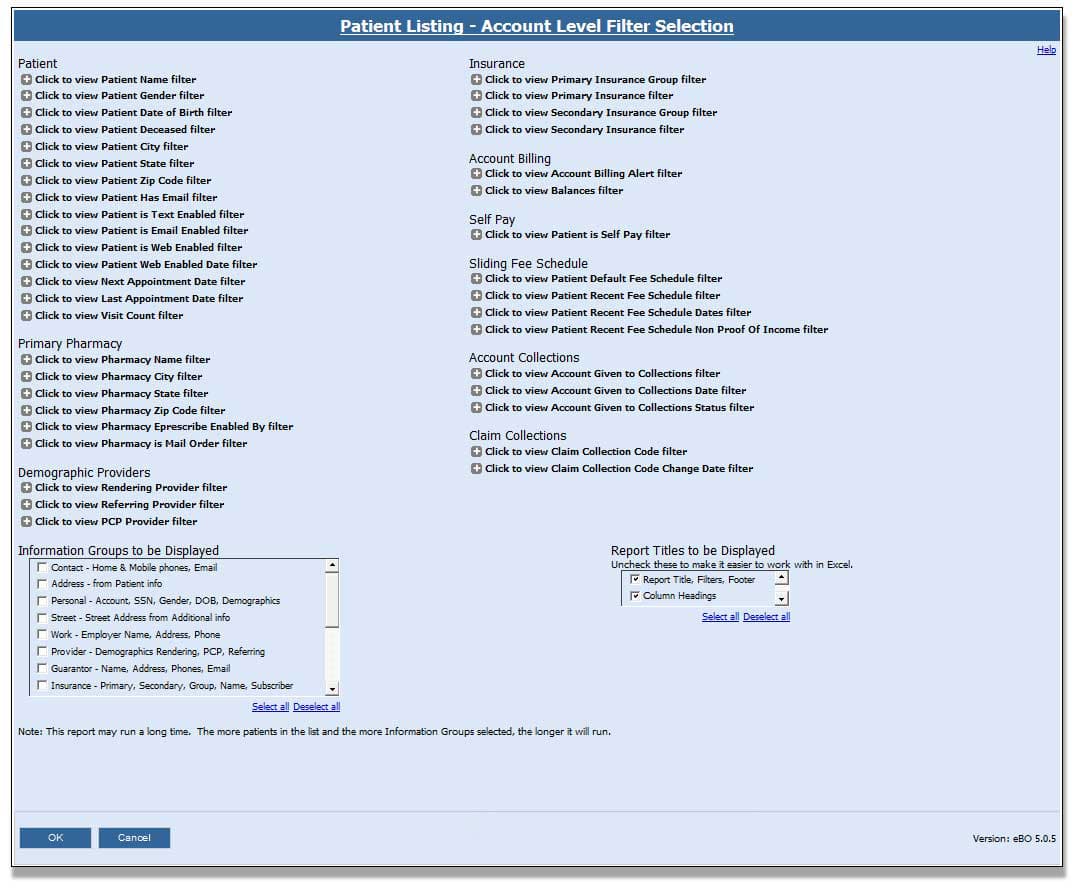
Patient Listing
Struggling to generate patient list for mailing, collections, patient satisfaction surveys, marketing campaigns, or detailed patient demographics? There are many ways to organize patient lists with this report.
$250.00
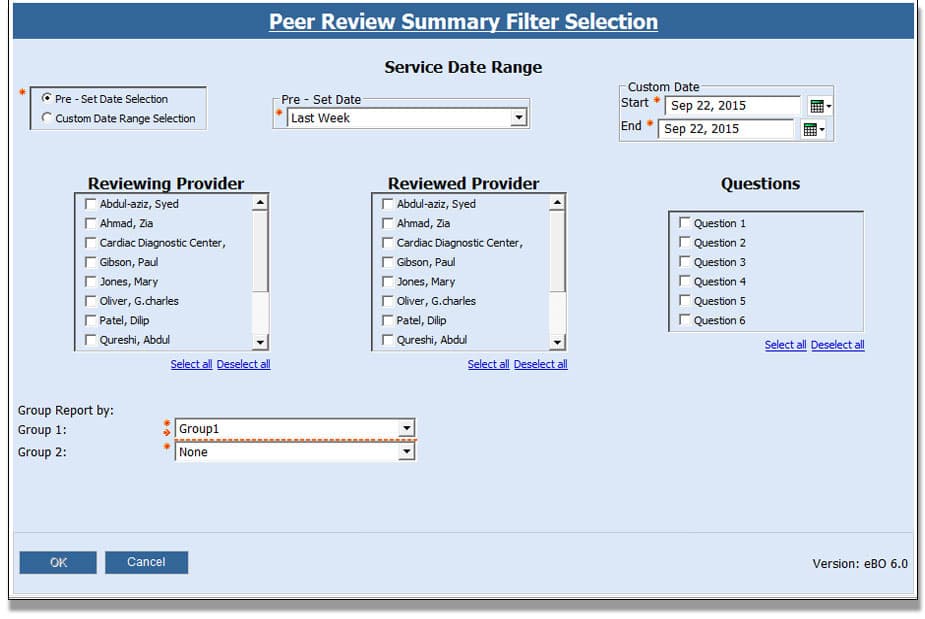
Peer Review
This report is helpful if you need to monitor or document peer review workload.
This report ensures that reviewing and reviewed providers are meeting goals and identifying which areas need more effort in the summary report and drill-down. You can also directly run the detail report to see Progress Notes’ details.
$250.00
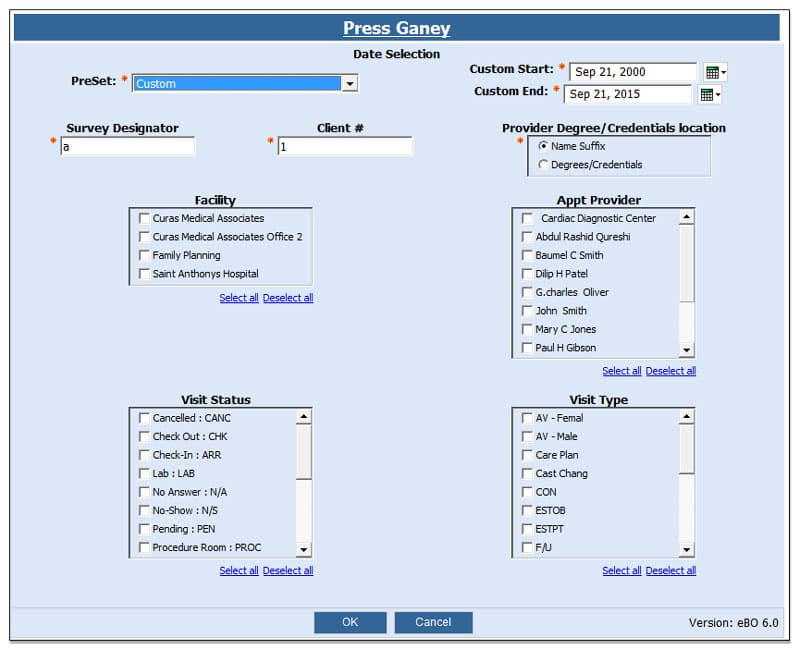
Press Ganey Survey
This report is helpful if you are having difficulty creating patient lists for surveys with contact information, patient demographic, and appointment details.
Creates list of patients with contact information in the standard Press Ganey format. Easily exported to MS-Excel or CSV. This report can also be be scheduled with preset dates including last week, month-to-date, last Month, etc.
$500.00
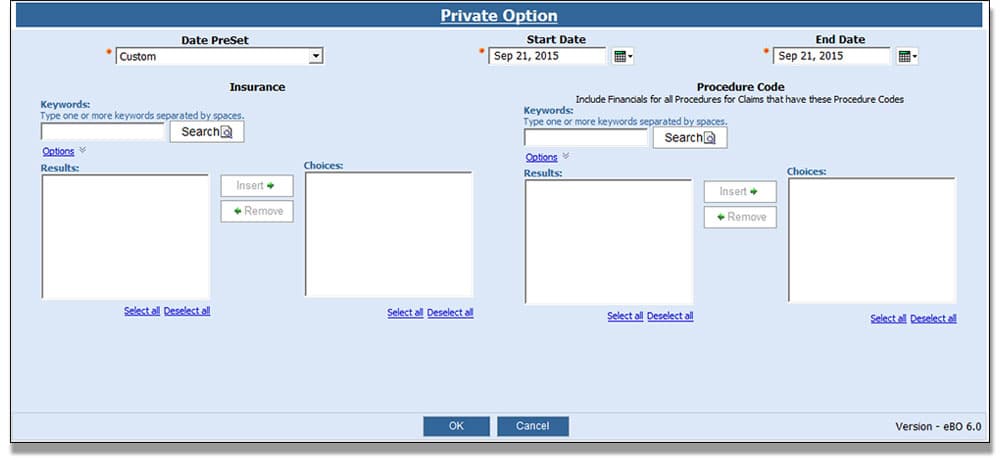
Private Option
This report is helpful if you are having difficulty reporting list of patients seen under the state’s Private Option insurance to DHS.
With the Private Option report you can create a list of patients seen in the format expected by AR-DHS. It can easily exported to MS-Excel or CSV and can be scheduled to run automatically.
$250.00
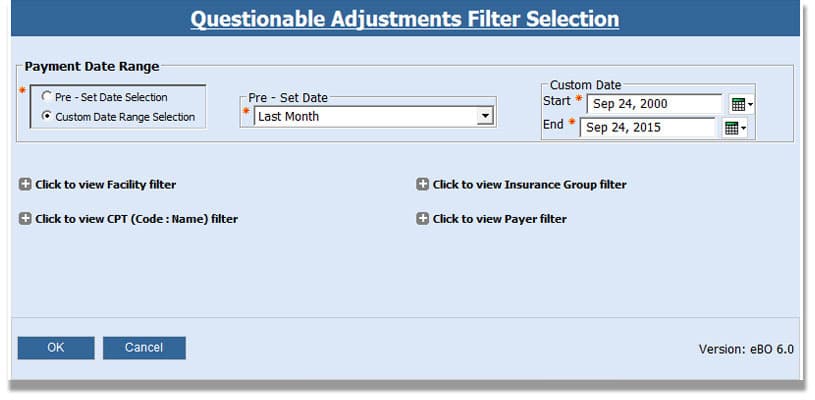
Questionable Adjustments/Denials
This report is helpful if you find ERAs that have an adjustment amount without a payment amount or list all non-contractual adjustment denials with an adjustment amount.
It can also help you identify payment details on payments with adjustment amount but no paid amount or adjustment amount with a Message Code, and it’s not CAS:45.
$250.00
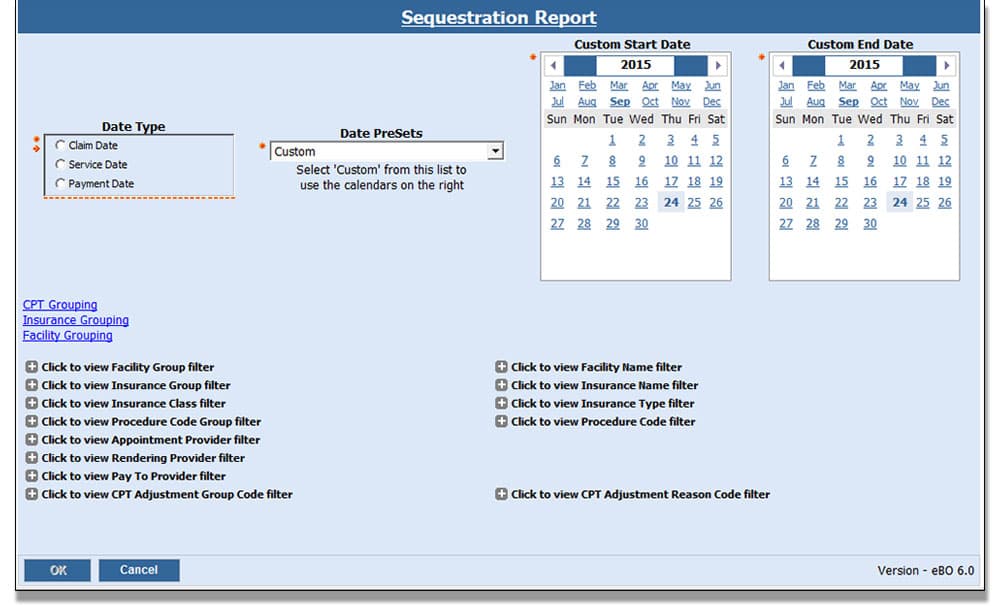
Sequester Report Bundle
This report is helpful if using CPT adjustments or ERA Remark Codes to record sequestration amounts. These reports will document the impact on your business.
This is a dual-report bundle that allows a practice to report on Medicare Sequester Adjustments using either CPT Adjustments or the ERA CAS code remarks.
For practices that are taking the time to enter CPT Adjustments, the CPT Adjustments report allows the practice to report on the exact Sequester Adjustments during a specified time period. If a practice has not been using the CPT adjustments but is ePosting ERAs, the ERA Remarks report allows practices to list claims with the corresponding CAS code for Sequester Adjustments. If the practice has been entering this amount in the Withheld field, they see these listed on the report.
$250.00
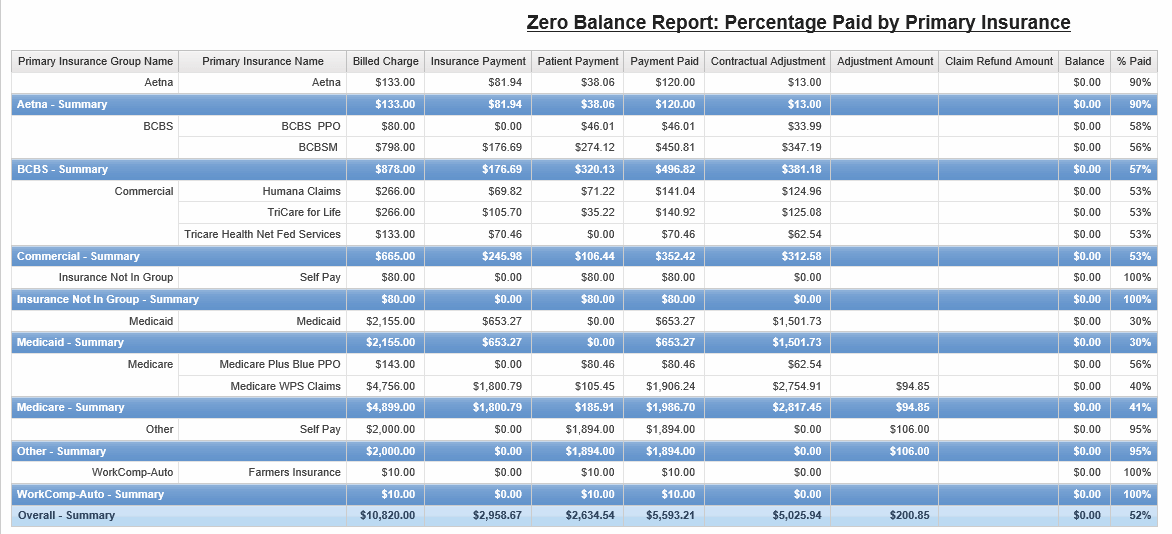
Zero Balance Report
The Zero Balance Report is used to determine the percentage paid by insurances on claims that have reached a zero balance. Determine your top reimbursing payers or use the information to forecast future income.
The report output summarizes charges, payments, adjustments and percentage paid by primary insurance group and primary insurance for all claims in the date range where the claim balance is zero.
A detail page is included of all the zero balance claims that make up the summary.
$450.00
Request More Information About Reports
Fill out the form below, and a member of our team will be in touch to further discuss your report needs.