For those FEW of you that read my blog for Mi7, don’t worry, these RCM360 blogs won’t be as technical. The blogs will, however, be just as witty and subject inappropriate as ever. I hope to bring some levity to your read while discussing some of the highest impacting topics related to the business of RCM on the eClinicalworks platform.
Well, since this blog is #1 of hopefully many, I would like to spend a little time with you discussing #1’s. This is not a blog about the best burger, pizza, or music, but I can give you my answers to all three. This is not about winning or our society’s desire to replace participation ribbons with ridiculous participation 3‐tier trophies. I read those top ten lists that come out on Yahoo and similar sites: top states to live, top investments, top beaches to visit, etc. Being #1 is not always the best. I did a search for “worst list”. The top 2 responses are: top 10 worst toys and top 10 worst movies. There are sites that are developed to give you worst lists. TIME even has their own best/worst lists.
RCM has its own list of best/worst lists. I came from a business consulting background and using technology to enable business processes. I am amazed at the inefficiencies I found in the standard RCM business process. I am especially interested in what the top denials (the ultimate RCM worst list) are for our clients when we first start their billing. By far, the #1 denial reason is patient eligibility.
I started to wonder, why is this the top denial reason? Why are all of these practices making this mistake? There are tools built into eClinicalworks tightly integrated with clearinghouses such as Trizetto to check patient eligibility for the next day’s appointments. There are automated jobs that can be created to do the check in batch without manually checking each patient. There are screens for monitoring eligibility statuses and failures. The eligibility status shows in the schedule screen. What is the break down?
I found varying levels of misconfiguration ranging from system setup to business process. In some clients, the eligibility is not set up at all. In some, it is not configured to check automatically. These things can easily be resolved, but the most difficult change is the business process for monitoring, determining correction, resubmission, and bringing in application support to address any issues that come up. This takes a diligent, informed user to make sure eligibility, even when configured properly, doesn’t remain the top denial reason.
RCM360 implemented a process where our staff review the automated eligibility results daily, addresses any issues, and resubmits the eligibility check to ensure coverage. We monitor these denials monthly to make sure we don’t need to review configuration, process, or user training.
Bottom line is you can’t just participate. You must be diligent. You must be engaged. You must take an interest in making sure that you are addressing all facets of the challenge. In this case, both the system and the process must be adjusted. Below are some items to consider in regards to eligibility.
- Do you have eClinicalworks integrated with a primary clearinghouse vendor such as Trizetto?
- Is eligibility set up and configured correctly? If you are not sure, do you have an expert you work with that can review it with you?
- What is your eligibility denial rate?
- How much revenue are you losing due to eligibility denials?
- What is your process for monitoring and correcting patient eligibility?
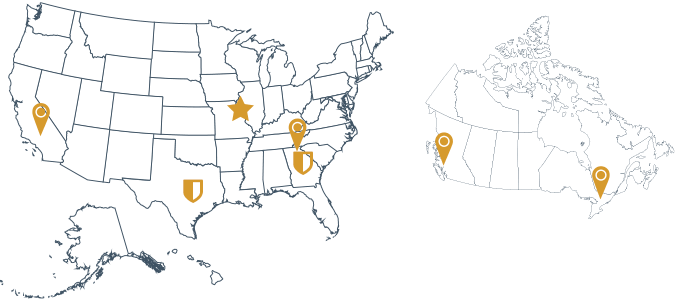
Be the best you can be. Be a winner not a participant. RCM360’s billing services can help you get on the right path to more efficient, faster collections by minimizing your denials and structured, regular insurance follow‐ups. Contact us to discuss your practice’s needs.