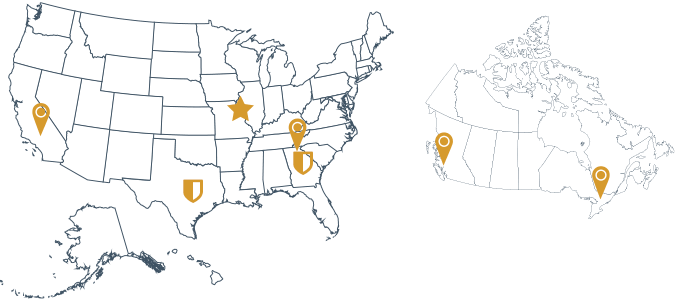
Effective Aug. 1, 2019, Anthem Blue Cross and Blue Shield began submitting their Electronic Remittance Advices (ERAs) directly to Availity. As a result, many practices that use the TriZetto clearinghouse platform are not receiving their Anthem Blue Cross and Blue Shield ERAs. This issue is specific to TriZetto-based practices in the following states: California, Connecticut, Indiana, Maine, New Hampshire, New York, Virginia, Colorado, Georgia, Kentucky, Missouri, Nevada, Ohio, and Wisconsin.
Affected providers are advised to contact Availity Client Services at 1-800-282-4548 and confirm that TriZetto Provider Solutions is set as the receiver for all Anthem Blue Cross and Blue Shield remittances or visit your STEM portal and initiate the re-enrollment process.
Strategic Enrollment Manager for TriZetto Provider Solutions
RCM360® utilizes Strategic Enrollment Manager (STEM), which is a portal within Madaket Health, one of the platforms we use to streamline payer enrollment. STEM provides users the ability to manage their payer enrollments more efficiently, saving time and eliminating administrative waste.
STEM allows practices that use TriZetto to:
- Enter admin, practice, provider, and payer information for enrollments
- View and complete all action items in one place
- View real-time enrollment status of payers
STEM is separate from the TriZetto client website, and clients who enroll will have separate login information for this system. New enrollees will receive a welcome email from support+stem@madakethealth.com, which will include a link to follow to activate their STEM account.
STEM is just one solution offered by RCM360 to streamline processes, eliminate errors, and optimize processing of medical claims to increase your revenue. Find out how we can increase your revenue and help you work smarter instead of harder. Contact us today.