Clean claims—and specifically first-time clean claims—are one of the most important indicators of high-performing revenue cycle management. Clean claims are defined by Medicare as claims that have ”no defect, impropriety, lack of any required substantiating documentation—including the substantiating documentation needed to meet the requirements for encounter data—or particular circumstance requiring special treatment that prevents timely payment.”
In short, clean claims have all the information needed for your practice to collect payment for services more quickly. Many practices leverage an electronic health records (EHR) system, like eClinicalWorks, for billing, which can both streamline and complicate the process. This blog will cover why clean claims are important to your business, common reasons for claims denials, and how to correct them.
Why Are Clean Claims Important?
The industry benchmark is 90% clean claims. If your practice doesn’t meet that benchmark, it can be overwhelming to tackle increasing the clean claims rate (CCR). There are a host of reasons to prioritize first-time clean claims, but the most obvious is that fewer days in accounts receivable means more revenue in a shorter amount of time. When claims are denied, 35% are never re-worked, meaning that revenue is never collected.
But where to begin? 90% of denied claims are a result of submission errors, and here are some of the most common reasons for claims denials:
- Lack of prior authorization. Authorization must be secured before services are performed, or you risk the claim being denied.
- Missing or incorrect information. This could be any piece of information along the way, from patient information to plan code to required modifiers.
- Procedure not covered by the insurer. Although this should require a simple verification, it still ranks as a top reason that claims are denied. Evaluate what’s covered by a patient’s plan prior to submitting the claim.
- Out of network provider. If the provider is not in-network, all or some of the claim can be denied.
- Multiple or duplicate claims. This happens when the same service, on the same day, by the same provider, for the same patient is filed more than once. In this event, each of the claims will be denied.
Address these by making sure you have the right people, process, and technology in place to mitigate claims denials. People are the biggest asset of any organization, and ensuring your team is adequately staffed and with ample training goes a long way toward improving CCR. Set processes in place to ensure that patient information is consistently reviewed and up to date in your EHR system.
How to Increase Clean Claims
In looking at the most common reasons for claims denials, most have a straightforward fix. Follow these steps to increase clean claims rate for your medical practice:
- Keep patient information updated. The right RCM or EHR provider should be able to set workflows in place to periodically check in with patients, so their information doesn’t go out of date. Adding this to your standard process—and standard technology—goes a long way to making sure CCR meets or exceeds 90%.
- Verify eligibility and benefits. This includes any precertification or referral requirements, as well as any filing limits or maximum benefits. Before a claim is filed, authorization, medical necessity, and benefits eligibility should be checked, and authorization should be received ahead of time.
- Code to highest specificity. Keep your codebook up to date, and code to the fifth digit whenever possible to reduce denials.
- Use technology to your benefit. Your EHR provider likely has an RCM component or works with a company that does. If you’re billing through eClinicalWorks, RCM360 has a standard process around the principles of simplicity, transparency, and open communication.
Keep Your Claims Clean
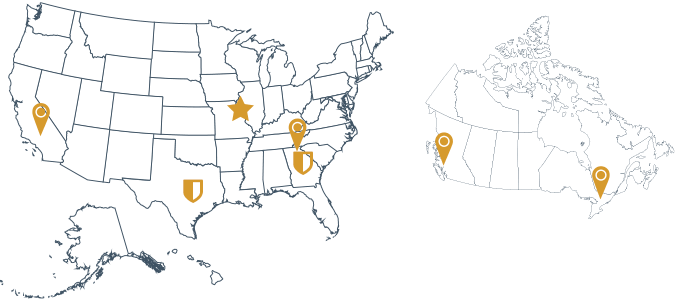
If your organization is meeting a 90% clean claims rate, congratulations! Meeting this benchmark likely means that you have strong RCM practices in place, but there may still be room for improvement. Continue to evolve your processes to increase CCR by following the tips provided above. And know that if you’re looking for RCM support in eClinicalWorks, RCM360, an Ero Health company, is here to help.